Piles
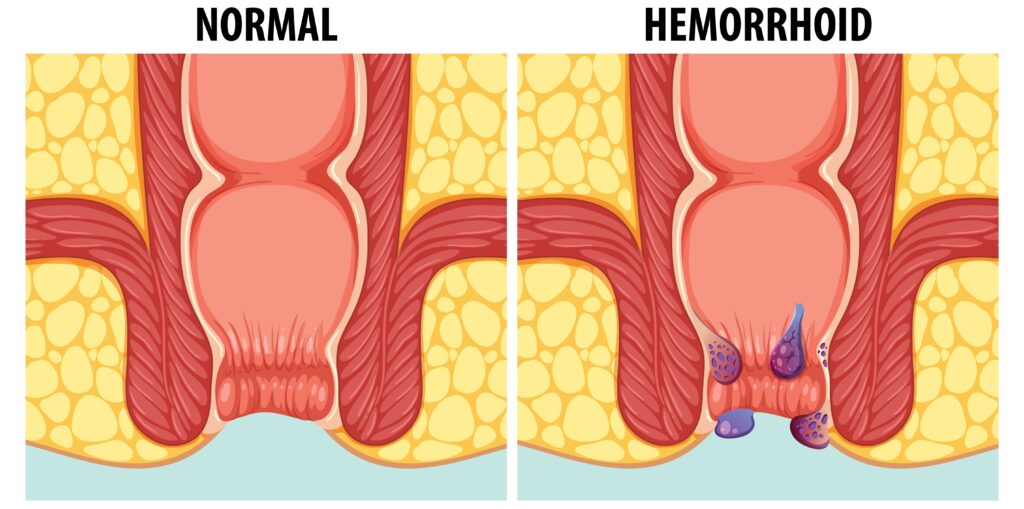
Piles, or hemorrhoids, are swollen veins in the lower part of the anus and rectum. They are common and can cause discomfort, pain, and bleeding, particularly during bowel movements. While not usually severe, understanding the importance of proper management and the available treatments is crucial to relieving symptoms and preventing complications.
Importance of Addressing Piles
Addressing hemorrhoids is important because they can significantly affect the quality of life. They can cause pain, bleeding, and itching that may result in discomfort and embarrassment. In some cases, they can lead to more serious conditions like chronic blood loss, anemia, and, rarely, an increased risk of colorectal cancer if associated with other symptomatic conditions.
Causes of Piles
Hemorrhoids are often linked to increased pressure in the lower rectum, which can cause the blood vessels in this area to swell and become inflamed. Common causes and risk factors include:
- Constipation and Straining: Frequent straining during bowel movements is a primary cause of piles.
- Prolonged Sitting: Sitting for long periods, especially on the toilet, can increase the pressure on the veins in the anus.
- Heavy Lifting: Regular heavy lifting can also increase abdominal pressure and contribute to hemorrhoids.
- Pregnancy: The increased pressure from the uterus on the abdomen, as well as hormonal changes, can cause hemorrhoids during pregnancy.
- Obesity: Excess body weight can increase the pressure on the abdominal and pelvic veins.
- Diet: A low-fiber diet can lead to constipation, which exacerbates hemorrhoids.
- Aging: Tissues in the lining of the anus may weaken and stretch with age, increasing the risk of hemorrhoids.
Treatments and Management Strategies
Treatment for piles depends on the severity of symptoms and includes home remedies, non-invasive procedures, and surgeries:
Home Remedies:
- High-fiber diet: Consuming more fiber can soften stools and increase their bulk, which helps reduce straining during bowel movements.
- Hydration: Drinking plenty of fluids supports bowel health and eases stools.
- Over-the-counter (OTC) creams and suppositories: These can offer temporary relief for swelling and discomfort.
- Warm baths: Sitting in a warm bath for 10 to 15 minutes can relieve discomfort.
Non-Invasive Procedures: For persistent or severe cases that do not respond to home treatments, doctors may recommend procedures such as:
- Rubber band ligation: A small band is placed around the base of the hemorrhoid inside the rectum to cut off its blood supply, causing it to wither and fall off.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid tissue to shrink it.
- Infrared photocoagulation: Infrared light is used to cause scar tissue, which cuts off blood supply to the hemorrhoid.
Surgical Treatments: In severe cases, surgery may be required:
Hemorrhoidectomy: This is the most effective and complete way to treat severe or recurring hemorrhoids.
- Hemorrhoid stapling: This is used primarily to treat internal hemorrhoids by cutting off the blood flow to the tissue.
